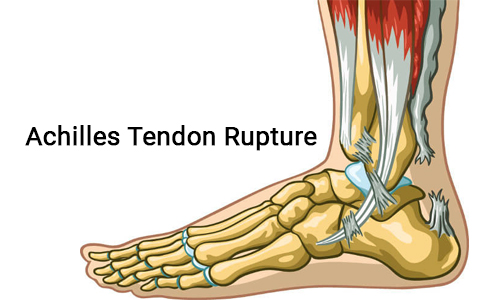
Achilles tendon ruptures are no longer considered to be career-ending injuries. Here’s how these injuries can be treated Despite being the thickest, strongest and largest tendon in the human body, Achilles tendon gets frequently injured. Achilles tendon ruptures (ATRs) mainly occur during sports activities. Moreover, their incidence has increased over the last few decades.

Achilles tendon ruptures (ATR) occur mainly during sporting activities as a result of a single high-load impact to the gastroc-soleus complex. The most common site of rupture is at the tendon itself, 2 to 6 cm proximal to its insertion. ATRs continue to be challenging to treat for both surgeons and athletes. They are debilitating injuries that can be season-ending and may require an extended period of rehabilitation prior to return to play (RTP).
These injuries are common in football, tennis, badminton, and jumping, among other sports. Degenerative changes are the most common histological findings in spontaneous tendon ruptures. These changes include high vascularity, collagen disorganisation and hypercellularity relatively close to the ruptured site. This injury may lead to reduced tensile strength as well.
While non-surgical management is an effective treatment strategy for non-athletes, elite athletes typically opt for surgical management to directly restore the native tendon anatomy, particularly muscle-tendon length in order to prevent long-term weakness. Surgery also reduces the risk of re-rupture, which has been demonstrated to be lower in surgically treated patients. Recent advances in operative techniques and functional rehabilitation protocols have enhanced athlete recovery following these injuries.
Diagnosis
History and clinical examination remain the mainstay of diagnosis for ATRs. Patients with ATRs often report sudden and severe pain in the Achilles tendon at the time of injury, with the feeling of being ‘kicked’ in the back of the calf or heel.
Physical examination reveals a palpable gap in the tendon proximal to its insertion. The Thompson test (calf squeeze) test is diagnostic. Compared to the contralateral side, when the calf is squeezed, there will be no passive plantarflexion of the foot on the injured side.
A single lateral X-ray of the heel is usually performed to exclude an avulsion type injury. Ultrasounds or MRI scans are not required if the diagnosis is made on clinical history and examination. These tests should be reserved for when the clinical findings are equivocal or for chronic tears.
Surgical Treatment
Surgical repair of ATRs generally involves outpatient surgery that is performed under general anaesthesia, accompanied with a nerve block to provide pain relief postoperatively.
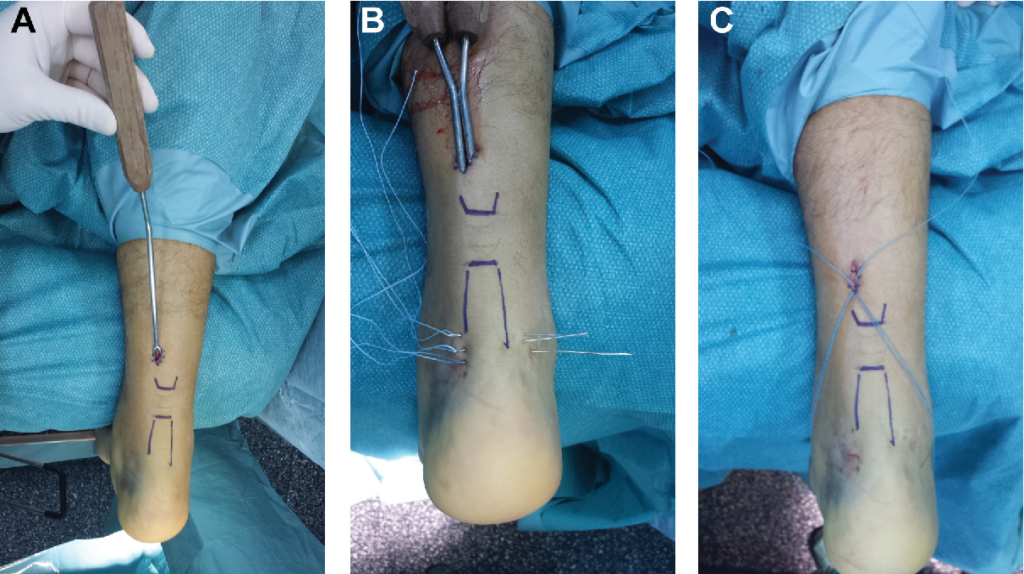
From a technical standpoint, surgery can either be performed through an open or minimally invasive approach. Both result in equivalent functional outcomes, however, studies have demonstrated that minimally invasive incisions (2cm or less) are associated with reduced wound healing complications.
More recently, both approaches have been augmented with additional suture anchor fixation in the calcaneus to reduce tension at the primary repair site. This augmentation increases the strength of the repair and can allow a more accelerated rehabilitation.
Rehabilitation
The current goal standard of rehabilitation after surgical management of ATRs is an accelerated protocol, with initiation of early weight bearing at the 2 week postoperative mark. Early weight bearing strengthens collagen fibres at the site of the repair and reduces the rate of re-rupture. Patients are transitioned from a cast to a fracture boot orthosis with heel wedges at week 2 and allowed to weight bear as tolerated. This boot is then removed by the 8 week mark and patients are transitioned to normal shoe wear.
With the advent of the augmented repair using calcaneal suture anchor fixation, this protocol has been further accelerated. Patients can commence a range of motion exercises within the first 6 weeks and anti-gravity treadmill running during this time. They are then transitioned into normal shoe wear by 6 weeks and can commence running by week 8 postoperatively. This has the potential to further reduce the time to RTP for athletes recovering from this injury.

Return to Play
RTP rates after surgical management vary between 61 to 100 per cent, with these rates varying based on the type of sport. Professional NBA players have the lowest RTP rates, due to the explosive plantarflexion demands required for basketball compared to other sports. Professional soccer, NFL and Major League Baseball players have significantly higher RTP rates than NBA players. Surgery for ATRs is evolving and comprises emerging techniques. ATRs should no longer be thought of as a career ending injury for professional athletes.
STORY CREDIT: (Authors’ Affiliation: Rothman Orthopaedic Institute, 925 Chestnut St, Philadelphia, Pennsylvania, 19103, United States of America)
Do you know?
South Africa spin bowler Keshav Maharaj required surgery and faced a long absence from cricket after rupturing the Achilles tendon in his left heel while celebrating a wicket in the second test against West Indies. Maharaj sustained a “complete rupture” of the tendon. The unusual injury saw Maharaj carried off the Wanderers field on a stretcher minutes after he got his second wicket in South Africa’s series-clinching 284-run win. He later reappeared on crutches and with his left foot in a moon boot. Maharaj threw his arms out and took one step as he set off on a celebratory run, then suddenly slumped to the floor and clutched his left leg. He lay on his stomach grimacing in pain as his teammates.

[/ihc-hide-content]